Abstract
Introduction:
Acquired somatic mutations in hematopoietic stem cells lead to myelodysplastic syndromes (MDS) and are also associated with accelerated atherosclerosis. In subjects without MDS, these mutations constitute a potent cardiovascular risk factor: clonal hematopoiesis (CH). In a previous analysis, we demonstrated that an MDS diagnosis was an independent risk factor for cardiovascular disease (CVD) compared to propensity matched non-cancer controls. CVD is the most common non-cancer cause of death in MDS, and rural residence has been independently associated with many CVD risk factors. However, there are no studies examining the association of geographic disparities and cardiovascular death in patients with MDS.
Methods:
We identified adult patients diagnosed with MDS between 2001 and 2016 using the Surveillance, Epidemiology, and End Results (SEER) database. MDS risk was classified as low, intermediate or high, using International Classification of Diseases for Oncology 3 rd Edition (ICDO-3) codes. Rural and urban populations were categorized using the US Department of Agriculture's Rural-Urban Continuum Codes (RUCC). Primary cause of death reported to State Registries (SEER COD recode) was used to estimate cause-specific survival, calculated from date of MDS diagnosis to date of CVD-related death. Cases with missing data on any key variable were excluded from analysis. SEER*Stat version 8.3.9 was used to calculate incidence rates. Chi-square and t-test were used to compare categorical and continuous variables, respectively. Survival analyses employed the Kaplan-Meier method and log-rank tests. Multivariable Cox-proportional hazards repression estimated the association of rural residence with CVD death adjusting for age, sex, race, ethnicity, MDS risk, and geographic location. SAS version 9.4 was used for statistical analysis.
Results:
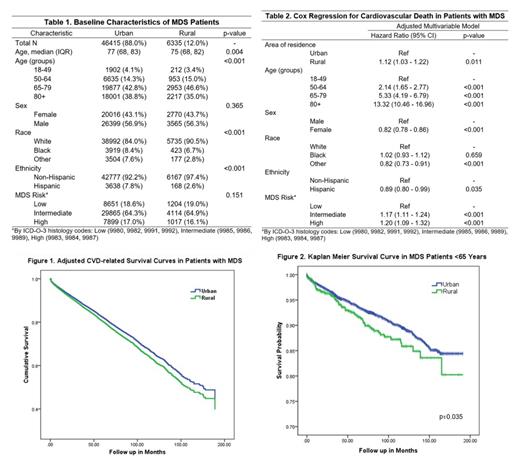
We included 52,750 patients with MDS, 56.8% were male and 84.8% were white. Low, intermediate and high histologic risk were seen in 18.7%, 64.4% and 16.9% respectively. Most patients were from urban areas (88%), however the estimated incidence rate for MDS was 6.7 per 100,000 per population at risk in both urban and rural populations. The rural MDS population was younger (median age 75 vs 77 years, p<0.004) and had a higher proportion of whites (90.5% vs 84%, p<0.001), but no difference in MDS risk distribution was noted by rurality (Table 1). Unadjusted analyses revealed a trend towards lower overall survival in the rural MDS population (24 vs 25 months, p=0.051). After adjusting for age, sex, race, ethnicity, MDS risk and area of residence, rural subjects with MDS had a 12% increased hazard (HR 1.12, 95%CI 1.03 - 1.22) for CVD-related death compared to urban subjects (Figure 1). Further, the adjusted HR for CVD-related death was 1.23 (CI95% 1.01 - 1.50) for those who lived in the most rural areas (RUCC codes 8 and 9, less than 2,500 urban population). Among young MDS patients (age<65), those residing in rural areas had a higher proportion of CVD-related death (6% vs 4.7%, p=0.031) and significantly shorter CVD-specific survival compared to urban patients (Figure 2). MDS histologic risk was also a significant factor in the multivariable model (Table 2). Compared to low risk MDS, patients with intermediate and high risk had adjusted HR for CVD-related death of 1.17 (95%CI 1.11 - 1.24) and 1.2 (95%CI 1.09 - 1.32), respectively. Other factors significantly associated with increased hazard for CVD-related death in the adjusted model were advancing age and male sex.
Discussion:
In a large population-based study, we found that rural area of residence is significantly associated with a higher burden of CVD-related death in subjects with MDS, after adjusting for demographic risk factors and MDS risk classification. Although aging is an important issue in rural areas, the geographical disparities in CVD-related death among MDS patients are not explained by age alone and the difference was notable in young MDS patients. These findings should prompt hematologists caring for patients with MDS from rural areas to rigorously evaluate and address CVD risk factors. As novel treatments improve cancer-specific survival in MDS, marginalized populations with different CVD risk profiles may be disproportionally affected by the cardiovascular risk from CH, which should be considered when developing MDS surveillance programs.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal